

Her GCS rapidly improved to 9, but the pupils remained fixed and dilated. Her Glasgow Coma Score (GCS) was 3 at the scene with fixed dilated pupils bilaterally (8 mm). A 50-year-old lady female cyclist fell over the handlebars of her bicycle at moderate speed and landed 8 ft away. Together with a literature review, these cases will help to outline four possible mechanisms of injury in mild to severe TBI and better explain the anatomical basis of 3cnP.
To elucidate the mechanism of injury underlying 3cnP, we present five exemplificative cases of isolated 3cnP in patients suffering severe closed TBI with documented Grade III DAI.


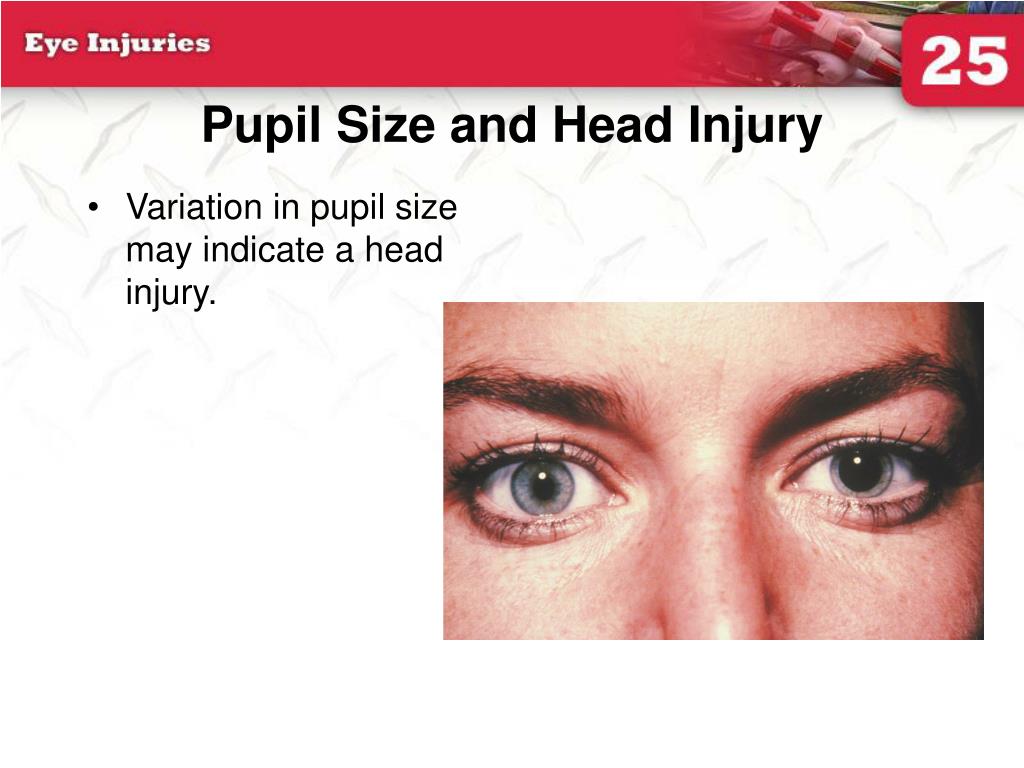
Furthermore, even when medical and surgical treatments are timely undertaken, 3cnP may not recover in fact, fewer than 5% of cases eventually show a complete recovery. CT scans are prone to artifacts and poor resolution in proximity to the brainstem, whereas very early MRI may not show DAI or may definitely underestimate the evolving cascade of secondary damage. Imaging alone can be ambiguous in defining the management. Fixed dilated pupils have thus historically been associated with a very poor prognosis in TBI. During the terminal stage of herniation, where the medulla is affected, the diffuse hypoxia continues to sustain mydriasis therefore, the damage becomes irreversible. This stage is also seen in uncal herniations. In later stages, when the midbrain is affected, pupils are moderately dilated (3–5 mm) and fixed. In this stage, pupils are normally small (1–3 mm) and reactive to light. In the early stages of central herniation, there is a diffuse bilateral hemisphere dysfunction due to decreased blood flow from increased intracranial pressure (ICP) and diencephalic dysfunction due to downward displacement. The size of the pupil and its reaction to light can indicate where the lesion is most likely to be located. An oculomotor injury can be the consequence of lesions located anywhere from the oculomotor nucleus in the midbrain to the termination of the third cranial nerve in the extraocular muscles within the orbit. Unfortunately, the pathological basis of isolated 3cnP has been poorly described in previous reports. In terms of clinical presentation, it can be found in combination with other cranial nerve deficits (particularly VI, V, and VI), can be unilateral or bilateral, and can be transient or permanent. Isolated 3cnP is very rare its incidence ranges from 8 to 16%, depending on the clinical series. Isolated 3cnP can be found in the absence of posttraumatic space-occupying mass lesion, yet it is often considered as a devastating prognostic factor in the context of diffuse axonal injury (DAI). 3cnP represents a worrying neurological sign because it is often associated with an expanding mass lesion, such as extradural or subdural haematomas. Third cranial nerve (oculomotor) palsy (3cnP) is seen in all grades of traumatic brain injury (TBI), either immediately after the traumatic event or evolving hours to days after it. Nonetheless, even when an overall good neurological outcome is achieved, recovery of isolated 3cnP is dismal, and only rarely the visual deficit completely resolves. Our experience corroborates data from the literature showing that, even in Grade III DAI, prompt recognition of isolated 3cnP can guide adequate treatment. Understanding the exact mechanism underlying the onset of 3cnP is key to provide an informed clinical decision-making to the patients and ensure their best chances of recovery. Through the analysis of five exemplificative cases and a thorough review of the literature, we identified four possible mechanisms leading to 3cnP: (1) a partial rootlet avulsion at the site of exit from the midbrain, representing a direct shearing injury to the nerve (2) a direct traction injury due to the nerve stretching against the posterior petroclinoid ligament at the base of the oculomotor triangle secondary to the downward displacement of the brainstem at the time of impact (3) a direct vascular compression as a result of internal carotid artery (ICA) dissection or pseudoaneurysm (4) an indirect injury caused by impaired blood supply to the third nerve in addition to the detrimental biochemical effects of the underlying brain injury itself. Third cranial nerve palsy (3cnP) following traumatic brain injury (TBI) is a worrying neurological sign and is often associated with an expanding mass lesion, such as extradural or acute subdural haematomas.


 0 kommentar(er)
0 kommentar(er)
